How Nurse Practitioners Can Start Their Independent Practice

What Is a Nurse Practitioner Private Practice?
Based on the latest projections from the Association of American Medical Colleges (AAMC), the U.S. could experience a shortage of between 17,800 and 48,000 primary care physicians by 2034 and a potential shortfall of up to 124,000 physicians overall. As a result, patients increasingly rely on nurse practitioners (NPs) for medical care.
The American Association of Nurse Practitioners (AANP) reports the significant role nurse practitioners play in the delivery of primary care today:
- 88.9% of nurse practitioners are certified in an area of primary care.
- 70.2% of nurse practitioners deliver primary care.
- 96.2% of nurse practitioners prescribe medications to patients, with those in full-time practice writing an average of 21 prescriptions per day.
Though some patients have resistance to nurse practitioners acting as primary care providers, many are using them when access to physicians is challenging. As advanced practice registered nurses, NPs possess robust skill sets and are qualified to provide a range of medical services.
NPs who want autonomy in operating their businesses while having greater freedom to provide medical care can start a nurse practitioner independent practice.
Patients can receive a range of primary and specialty care services from a nurse practitioner private practice, similar to those offered at a physician’s office. A nurse practitioner may provide a scope of services, depending on the practice:
- Patient assessments and diagnoses
- Diagnostic and laboratory tests
- Prescription and management of treatment plans
- Prescription of medications
- Care coordination with other health care professionals
- Patient and family counseling on healthy living and how to manage illnesses and injuries
An NP offers patient-centered care, which entails a comprehensive understanding of a patient’s condition and lifestyle to provide tailored treatment.
Scope of Practice
While many nurse practitioners work autonomously in private practice, some states limit the scope of services they can provide independent of physician oversight or involvement. NP practices could offer full, reduced, or restricted services, depending on practice location.
Full Practice
Nearly half of the U.S. states, plus Washington, D.C., grant nurse practitioners a full practice designation. This status conveys that, in most cases, they can work independently if meeting certain criteria (such as state licensure requirements). In these states, nurse practitioner independent practices can provide a range of services without physician oversight, including patient exams; performing, ordering, and interpreting diagnostic tests; prescribing medication; and managing treatment plans.
Reduced Practice
Reduced practice states limit the ability of NPs to engage in at least one element of practice without physician oversight. In many cases, they can diagnose and treat patients, but require physician involvement—often in the form of a collaborative practice agreement—to prescribe medication.
Restricted Practice
In restricted practice states, an NP generally needs full physician oversight or supervision to care for patients. California, Florida, and Texas are among the 11 restricted practice states.
Role of NPs in Underserved Areas
NPs play an even more vital role in rural and inner-city areas with limited availability of physicians. According to the AAMC, roughly 60% of the 7,200-plus federally-designated health professional shortage areas are in rural areas. For many of the people who live in these areas, NPs are the main source of primary care.
A report from the Journal of the American Academy of Physician Assistants speculated that the nation’s projected physician shortages could be greatly reduced—and potentially erased—if the contributions of nurse practitioners and physician assistants were more accurately accounted for in health care workforce projections.
Many states that grant full practice rights to NPs are in rural and remote parts of the country, such as Alaska, Montana, Wyoming, and the Dakotas. Studies have shown that in full practice states, NPs are more likely to practice in underserved areas, according to AANP, often leading to improved access to care and lower costs for patients. States that limit the ability of NPs to practice, however, tend to experience more primary care shortages, greater geographic health care disparities, and higher rates of chronic disease.
How to Start a Nurse Practitioner Private Practice
Earning an advanced degree is essential for NPs, whether operating a practice or working in a hospital. A master’s degree with a focus on a nurse practitioner practice provides health care professionals with foundational knowledge and clinical experience to prepare for certification in their chosen specialty. An advanced degree and certification also are necessary for state licensure.
Those interested in learning how to start a nurse practitioner private practice should follow these essential steps.
Obtain State Licensure
NPs must hold an active registered nursing license in their practicing state, along with an advanced practice registered nursing license.
Get a DEA Number
NPs must register with the Drug Enforcement Administration (DEA) to administer, prescribe, or dispense controlled substances.
Negotiate Hospital Privileges
NPs often admit patients to the hospital. To make this process as seamless as possible, NPs need to negotiate certain privileges with the hospital, which allows them to admit and visit patients.
Establish Insurance Reimbursement Contracts
Establishing contracts with third-party insurance companies is critical for an NP independent practice to get compensated for provided services. NPs must obtain credentialed from insurance companies to receive reimbursement, which can take time for new practices and potentially delay payment. Additionally, reimbursement rates for NPs may vary by insurance. For example, Medicare reimburses NPs at 85% of the physician pay rate. NPs must be aware of the rates that apply to them.
Finance Startup Costs
Starting a private practice can be expensive, so determining startup financing is crucial. NPs can finance their practice with a business loan from a commercial lender, establishing a line of credit, or applying for a loan from the U.S. Small Business Administration.
Create a Billing System
NP private practices cam face issues with billing and collections, particularly since payments often are delayed for new practices. An effective billing system can alleviate these issues and allow NPs to focus on the most important aspect of their job: caring for patients.
Craft a Business Plan
A well-crafted business plan provides a road map for an NP to build, operate, and grow a private practice. A business plan helps NPs think through key components of the operation, forecast growth and serve as an effective tool for attracting investors or seeking other forms of financing.
Find a Location
Location is another important consideration. NPs should ask themselves what services they’re going to provide and how much space they need to do it while considering future growth.
Resources for Starting a Nurse Practitioner Private Practice
Nurse practitioners looking to open a private practice may have lots of questions such as “How much money do I need to get started?” or “What kind of location do I need?” Multiple resources can help answer them.
- Write Your Business Plan, U.S. Small Business Administration: This resource can help NPs craft a business plan for their practice and answer fundamental questions about their business.
- Nurse Practitioners: Opening Your Own Practice, Minority Nurse: This resource guides NPs considering opening a practice through the process, tackling questions related to location, staffing, and marketing.
- How to Finance Your Practice from Startup to Growth, Nurse Practitioner Business Owner: This resource provides answers to critical questions on financing an NP independent practice.
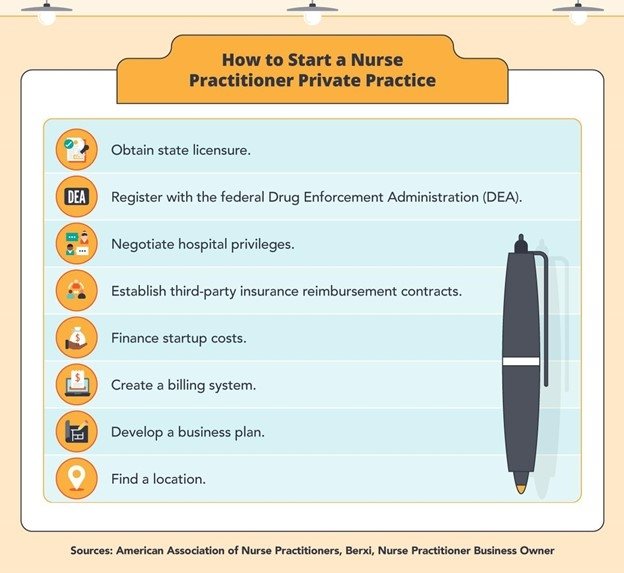
Here are eight steps to take before launching your practice: obtain state licensure, register with the federal Drug Enforcement Administration (DEA), negotiate hospital privileges, establish third-party insurance reimbursement contracts, finance startup costs, create a billing system, develop a business plan, and find a location.
Types of Nurse Practitioner Private Practices
Nurse practitioners can specialize in different areas of care. Among the more common nurse practitioner private practices are those specializing in psychiatric, family, or acute care.
Each of these specialties provides different services, requiring that NPs in these fields possess unique skill sets.
Psychiatric Nurse Practitioner Private Practice
Psychiatric nurse practitioners assess and diagnose patients’ mental health needs and provide treatment options. They may prescribe medication, provide therapy for patients with mental health disorders or substance abuse issues, and work with their families.
These NPs work in various settings including private practices, hospitals, community health centers, and nursing homes. A psychiatric nurse practitioner private practice promotes mental health in many ways:
- Working with children who experienced traumatic events.
- Assisting older patients dealing with Alzheimer’s disease or dementia.
- Helping soldiers dealing with post-traumatic stress disorder.
Private practice is one of the top practice settings for psychiatric NPs along with behavioral health/addiction clinics and psychiatric mental health facilities.
Requirements for a Psychiatric Nurse Practitioner
A psychiatric NP must possess at least a master’s degree, preferably with a concentration in mental health.
Additionally, psychiatric NPs must obtain the Psychiatric-Mental Health Nurse Practitioner-Board Certified (PMHNP-BC) credential from the American Nurses Credentialing Center (ANCC) before they can open a practice. Possession of a registered nursing license and an advanced degree from an accredited psychiatric-mental health nurse practitioner program are required to sit for the ANCC certification exam.
The proper educational background and training can help psychiatric NPs develop certain skills and abilities considered essential for this role:
- Communication. Psychiatric NPs must communicate effectively with patients to understand the nature of their mental health needs and prescribe appropriate treatment.
- Compassion. To properly treat mental health, NPs need to understand and be sensitive to patients’ individual circumstances, including their social and cultural background and that their conditions don’t define them.
Resources: Psychiatric Nurse Practitioner Private Practice
With roughly 20% of U.S. adults—and 17% of children ages 6 to 17—experiencing some form of mental illness, according to the National Alliance on Mental Health (NAMI), the work of psychiatric nurse practitioners is vital. Individuals interested in this career path can learn more through the following resources:
- About Psychiatric-Mental Health Nursing, American Psychiatric Nurses Association: This resource provides basic information about the psychiatric NP role.
- Frequently Asked Questions About Psychiatric-Mental Health Nurses, American Psychiatric Nurses Association: This resource answers common questions about psychiatric NPs, detailing what they do, where they work, and describing how to become one.
- Are You Considering a Career as Psychiatric Mental Health Nurse Practitioner?, American Association of Nurse Practitioners: This resource defines the role of a psychiatric NP and provides information on how to obtain certification.
Family Nurse Practitioner Private Practice
A family nurse practitioner private practice treats patients of all ages, from infants to seniors. Family NPs provide a wide range of primary care services:
- Physical exams
- Diagnostic tests
- Prescription of medications
- Treatment of acute or chronic illnesses and injuries
Family NPs also promote healthy lifestyles and educate patients on disease prevention. In addition to private practice, family NPs work in community health centers, hospitals, and universities.
Requirements for a Family Nurse Practitioner
As with other NP roles, family NPs must hold at least a master’s degree in nursing, ideally in family care. The coursework and clinical experience that an advanced nursing program provides can help family NPs develop the necessary skills to provide comprehensive care to diverse patient populations, such as:
- Interpersonal skills. Family NPs work with patients of all ages from many different walks of life, as well as their families. Connecting with patients is critical to help them understand diagnoses and adhere to treatment.
- Collaboration skills. Family NPs often work with other health care professionals, including other nurses and physicians, to coordinate patient care.
Family NPs also need to obtain a Family Nurse Practitioner Certification from the ANCC or AANP.
Resources: Family Nurse Practitioner Private Practice
Family care is the most common specialization among nurse practitioners, with nearly 70% of NPs holding their primary certification in this area, according to AANP. Those interested in pursuing a career as a family NP can explore the following resources:
- Are You Considering a Career as a Family Nurse Practitioner?, American Association of Nurse Practitioners: This AANP resource provides information on the family NP role, with some key statistics, as well as links to career resources.
- Family Nurse Practitioner (FNP), American Academy of Nurse Practitioners Certification Board: This resource discusses the AANP family NP certification exam.
- Family Nurse Practitioner Certification (FNP-BC), American Nurses Credentialing Center: This resource provides information on the ANCC certification exam, including the contents of the test and eligibility requirements.
Acute Care Nurse Practitioner Private Practice
Acute care NPs provide medical care to patients with acute and often chronic medical conditions. Many acute care NPs focus on adult-gerontology acute care, primarily working with older patients in settings such as nursing homes, emergency rooms, and trauma units.
They provide a range of services, including patient exams; ordering, performing, and interpreting tests; making diagnoses; and prescribing medication or treatment.
An acute care NP private practice specializing in adult-gerontology also may provide palliative care, improving the quality of life for patients with serious, long-term health conditions.
Requirements for an Acute Care Nurse Practitioner
Adult-gerontology acute care nurse practitioners (AGACNP) must obtain an advanced degree in nursing. These programs generally require one to three years of experience working as a registered nurse in an acute care setting.
The curriculum and clinical experience provided by a master’s or other advanced nursing program can prepare students for the AGACNP certification exam, administered by either the ANCC or the American Association of Critical-Care Nurses (AACN).
Education and certification can help AGACNPs develop competencies with:
- Acute care diagnoses and interventions.
- Technology used for advanced diagnostics, such as an electrocardiogram (ECG) and X-rays.
- Disease and pain management skills.
Resources: Acute Care Nurse Practitioner Private Practice
As the population of the country ages and people live longer with chronic and acute health conditions, the health care industry will need AGACNPs to care for them. Individuals interested in this career path can learn more through the following resources:
- “The Role of Adult Gerontology Acute Care Nurse Practitioners,” American Nurse: This resource examines the role of AGACNPs, providing information on the educational background and job outlook for the profession.
- Are You Considering a Career as an Adult-Gerontology Acute Care Nurse Practitioner?, American Association of Nurse Practitioners: This resource explores the work of AGACNPs, as well as their responsibilities and work environments, and provides information on certification.
Typical Nurse Practitioner Private Practice Salary
Though generally competitive, the median annual salary for nurse practitioners in private practice and other settings may vary depending on several factors, including experience and location. According to the U.S. Bureau of Labor Statistics (BLS), the median annual salary for NPs was $111,680 in May 2020.
The BLS also tracks salary figures for the position in states with the highest employment levels of nurse practitioners: California, New York, Texas, Florida, and Ohio. Because the job market is more competitive, salaries in some of these states are higher than the national average for the role.
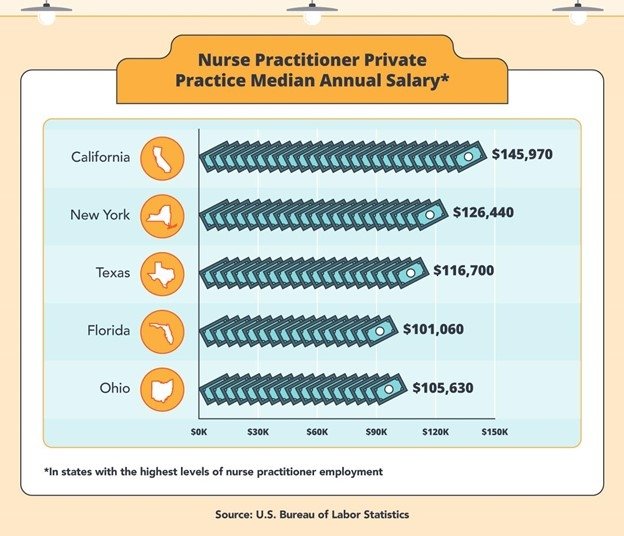
California is the state with the highest level of nurse practitioner employment, with a median nurse practitioner salary of $145,970. It is followed by New York ($126,440), Texas ($116,700), Florida ($101,060), and Ohio ($105,630).
Nurse Practitioner Salaries by Specialty
Salaries for nurse practitioners also may vary based on specialty. The following are the median annual salaries for family, psychiatric, and acute care nurse practitioners, based on August 2021 data from PayScale.
- Family nurse practitioner: $97,000
- Psychiatric nurse practitioner: $111,600
- Acute care nurse practitioner: $103,900
Independence in Nursing Practice
As the population ages and the health care needs of Americans grow, the role of nurse practitioners will become even more vital. Additionally, the nation’s ongoing physician shortage increasingly positions nurse practitioners as alternate primary care providers.
Starting a nurse practitioner independent practice allows NPs to build a network of referrals, gain greater independence caring for patients, and the freedom to run their business and potentially earn more income.
Infographic Sources:
IG #1 Sources:
How to Get Information About Obtaining a DEA Number, American Association of Nurse Practitioners
How to Open Your Own Private Practice as a Nurse Practitioner, Berxi
10 Steps to Starting Your Independent Nurse Practitioner Practice, Nurse Practitioner Business Owner
IG #2 Sources:
Occupational Employment and Wages, May 2020, 29-1171 Nurse Practitioners, U.S. Bureau of Labor Statistics
Explore Norwich University
YOUR FUTURE STARTS HERE
- 30+ On-Campus Undergraduate Programs
- 16:1 Student-Faculty Ratio
- 25+ Online Grad and Undergrad Programs
- Military Discounts Available
- 22 Varsity Athletic Teams
